The Realities of Living with Binge Eating Disorder
A conversation we need to have about binge eating disorder
Did you know that Binge eating disorder (BED) is actually the most common eating disorder, yet it’s often the least recognised and the least treated?
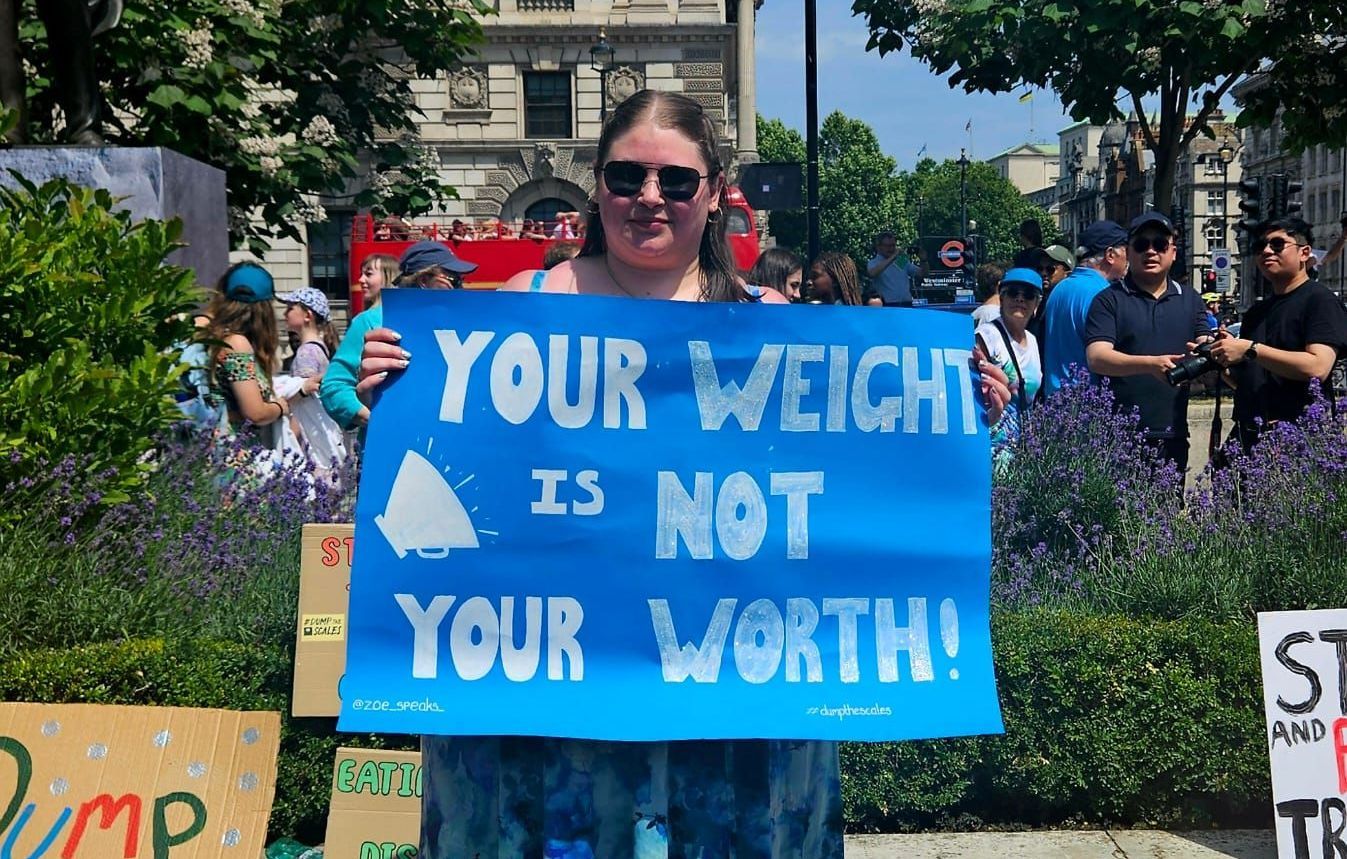
Society’s weight-focused lens means that many people living with BED go unnoticed, unsupported, and misunderstood, with lots of stigma and assumptions that when you ask someone about their experience really aren't true.
In this week’s Full of Beans podcast episode, Han sat down with Zoe Hazel, a mental health advocate, campaigner, and public speaker with lived experience of binge eating disorder, bipolar disorder, and borderline personality disorder.
Zoe’s honesty cuts through the noise of misunderstandings and shines a light on the realities of living with BED. She shares her journey from childhood secrecy to adult self-compassion, and she doesn’t shy away from naming the stigma that shaped her experience.
When binge eating begins in silence
Zoe recalls first engaging in binge eating at just 11 years old. For her, food started as a form of control and comfort in a life that felt both strict and chaotic.
She describes the secrecy (buying food from the shop with her pocket money and hiding wrappers under her bed), and the overwhelming shame that followed a binge. Like so many people with BED, she learned to mask her struggles, especially as she was in a body that society deemed “healthy” at the time.
“I didn’t even know binge eating disorder existed — I just thought I was the problem.” – Zoe
“Eating disorders thrive in silence. When you take away that secrecy, it doesn’t make the problem go away — but it makes it harder to hide.” – Zoe
Restriction: the hidden side of binge eating disorder
Many people think BED is all about overeating, but Zoe makes it clear there’s another side:
restriction.
“There’s just as much restriction with binge eating disorder as there is with anorexia or bulimia — it’s just not visible to most people.” – Zoe
For Zoe, restriction often came in cycles:
- Limiting food intake for days to “make up” for a binge.
- Exercising beyond her body’s limits to try to “compensate.”
- Feeling guilty for eating at all, even small amounts.
This cycle of
restrict → binge → guilt → restrict is what keeps BED in motion. The restriction lowers her body’s energy reserves and increases the biological drive to eat — making another binge feel almost inevitable.
“People only see the weight or the eating. They don’t see the restriction, the over-exercising, or the shame.” – Zoe
The truth about BED
Zoe addresses some of the biggest myths about BED:
- Myth: BED is simply about a lack of willpower.
Truth: BED is a complex mental health condition, often rooted in trauma, emotional regulation difficulties, and long-standing behavioural patterns. - Myth: Only people in larger bodies binge eat.
Truth: BED affects people of all sizes, ages, genders, and backgrounds. Body size alone does not reveal someone’s eating behaviours. - Myth: Treatment is just about eating less.
Truth: Recovery focuses on understanding emotional triggers, building coping strategies, and healing your relationship with food — not restriction.
Bipolar disorder’s impact on eating patterns
Zoe also lives with bipolar disorder, and she’s seen firsthand how it complicates her eating behaviours.
During depressive episodes, she often turns to food for comfort. Low mood and energy make cooking feel impossible, so takeaways or convenience foods become the easiest option.
In elevated (hypomanic) states, the opposite happens: she loses her appetite entirely and can go long periods without eating. Both extremes disrupt her eating patterns and feed into the BED cycle.
“When I’m depressed, I eat more for comfort. When I’m in hypermania, I don’t feel hunger at all. Either way, my eating disorder gets triggered.” – Zoe
Being diagnosed without being treated
Zoe wasn't diagnosed with BED in 2019... nearly two decades after her symptoms began. When she was finally diagnosed by her community mental health team, she was told there were no treatment services available in her area.
That was the end of the conversation.
“Binge eating disorder is treated like comfort eating taken too far, instead of a serious mental health condition.” – Zoe
Instead of receiving compassionate care, Zoe was met with weight stigma in healthcare. She explains that while weight loss in a smaller body would have triggered concern, weight gain in a larger body only brought blame and shame.
“If I’d lost weight suddenly, I’d have been asked if I was okay. But when I gained weight, no one asked — they just assumed I was to blame.” – Zoe
This is a reality many with BED face: diagnosis without support, left to Google their way through recovery. For Zoe, it highlighted the urgent need for systemic change in how eating disorders are treated, especially those that don’t fit society’s narrow image.
Finding recovery tools without formal treatment
Without professional BED-specific support, Zoe has had to develop her own strategies:
- Speaking openly about urges and struggles with trusted friends.
- Practising self-compassion instead of shame after a binge.
- Pausing before acting on an urge — writing down what she wants to eat and taking time before deciding.
She’s clear: these tools don’t make her “perfect” or “cured”, but they do give her moments of choice and self-care in a cycle that can feel relentless.
“I’m not perfect. I’m still in recovery. But every time I pause, every time I talk about it instead of hiding it — that’s a win.” – Zoe
Why Zoe’s story matters
For anyone living with binge eating disorder, Zoe’s story is a reminder that:
- You are not alone.
- Your struggles are valid, regardless of your body size.
- Shame and secrecy keep BED in the shadows — talking about it helps break its hold.
- Recovery isn’t linear, but every small step counts.
If you’re struggling, you deserve support — and it’s okay to advocate for yourself until you find it.
Listen to the full conversation
Zoe’s episode is available now on Spotify, Apple Podcasts, and all major platforms. Hear her full story, her insights on stigma, and the practical ways she supports herself without formal treatment.
Sending positive beans your way, Han 💛